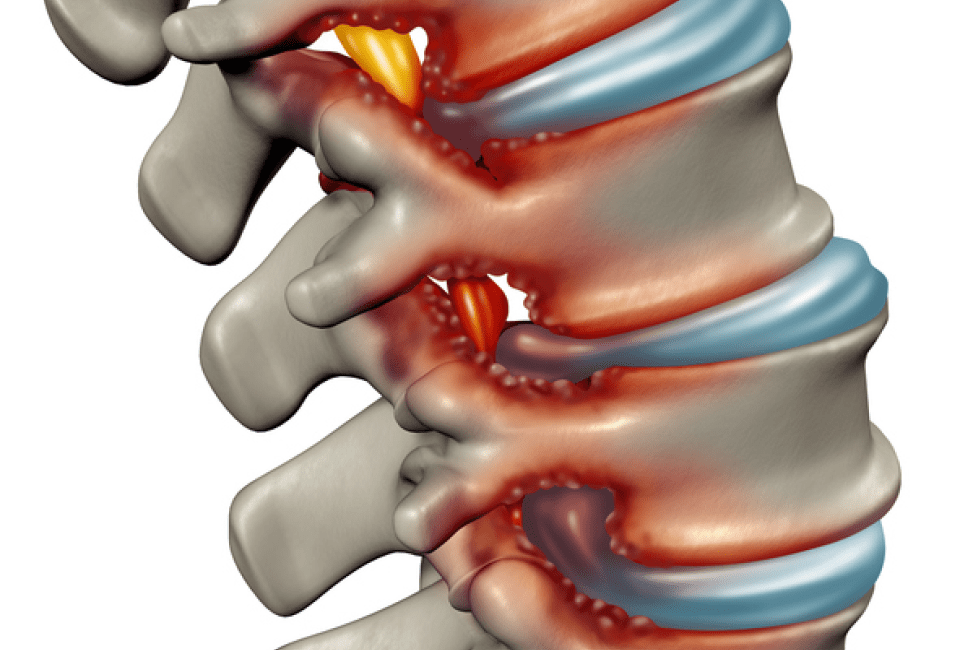
What is foraminal stenosis?
Foraminal stenosis is a narrowing of the intervertebral foramen which are narrow openings along your spine. In a way, they are like conduits that protect the wiring of your nervous system as it winds through the skeletal system of the spine. These delicate nerves or ganglion run from your spinal cord to your extremities. Each of the 23 intervertebral discs of your cervical, thoracic and lumbar spine are positioned adjacent to the openings of the foramen. Therefore, if one of your discs slips or herniates, the foramen openings could be narrowed which will compress nerves and activate pain. Nature has designed the spine to be rugged, and compact so there is not a lot of leeway in the design of these openings.
What causes foraminal stenosis?
The most common cause of foraminal stenosis is degenerative disc disease caused by aging, osteoarthritis, bone spurs, slipped vertebra (spondylolisthesis), cysts, tumors, damaged facet joints, enlarged ligaments, scoliosis and rarely Paget’s disease and genetic conditions such as dwarfism. Foraminal stenosis can also be caused by an athletic injury or any traumatic event such as a car accident.
What are the symptoms of foraminal stenosis?
The nerves running through the foramen connect to your extremities. The pain that is generated is similar to the pain of a herniated disc which means it radiates from your extremities and is called radiculopathy. If you have tingling pain along your buttocks, hips, legs, and feet the location of the stenosis is in your lower spine (lumbar). You may also experience weakness in your legs and numbness. If the pain that you are experiencing is in your shoulders, arms or hands, the location is in your upper spine (cervical).
Your treating physician may require additional information to pinpoint the source of the stenosis and may suggest using X-rays, MRIs, CT scans or electrophysiological tests. Information is key when it comes to identifying the biomechanical causes of your back pain.
How is foraminal stenosis treated?
The best way to characterize foraminal stenosis is as a pinched nerve. The objective of the conservative, non-surgical treatment plan is to naturally decompress the nerve over time.
If your doctor has identified your condition as lumbar foraminal stenosis, he or she may suggest that you work with a physical therapist and focus on lumbar extension and flexion exercises to stretch your nerves in much the same way as you would stretch a muscle to tone it.
If your problem is cervical foraminal stenosis, the conservative non-surgical treatment program may include over the counter anti-inflammation medicines, physical therapy and at-home traction units. For some cases, your doctor may suggest central and transforaminal epidural steroid injections which will help reduce inflammation and pain. Some physicians may prescribe opioid-based pain relievers.
Dr. Melamed is a great believer in integrative medicine techniques which may include yoga, acupuncture and chiropractic treatments. His conservative treatment plans are opioid-free and use diet and lifestyle assessments to help patients relieve back pain naturally. Most patients experience pain relief after two to three months of treatment without surgery or opioids.
A small percentage of patients may not respond to the conservative approach and may require surgery. Perhaps the optimal treatment is foraminal decompression using microsurgery techniques to reduce damage to soft tissue, muscles and bone structures. Some cases with spinal instability may require more intensive surgical solutions such as artificial disc replacement or disc fusions both of which are more invasive(1).
You Can Live a Life Free of Back Pain
Click on the “Make An Appointment” button at the top of this page, or call Dr. Melamed’s office for more information. There is no better time than today to start the journey to a life without back pain. Call us at 424-21-SPINE.
References:
1: Lumbar Foraminal Stenosis, Orita, S., Inage, K; Eur J Orthop Surg Traumatol. 2016 Oct;26(7):685-93. doi: 10.1007/s00590-016-1806-7. Epub 2016 Jun 18.